What Happens During an Oral Cancer Reconstruction Surgery
Reconstruction surgery after oral cancer might mean moving tissue or bone from somewhere else in the body to the mouth. Doctors do this with a special surgery called microvascular surgery. They carefully connect tiny blood vessels under a microscope to make sure the new tissue gets enough blood. This helps the repaired area heal properly.
This kind of surgery is commonly done to fix things in the mouth that are important for eating, talking, and swallowing. Sometimes, if teeth are taken out, dental implants might also be needed.
Soft Tissue Reconstruction
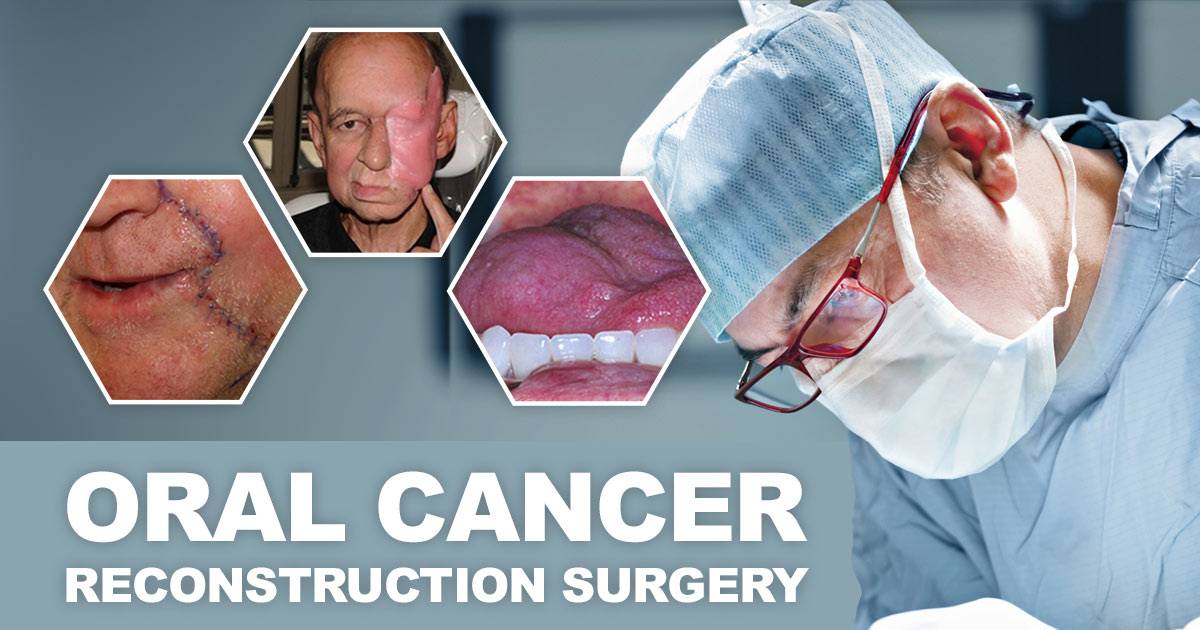
Doctors can rebuild soft tissue in different ways after cancer. They might use skin from another part of the body and attach it to the affected area (skin grafts), or they could move tissue nearby (local flaps) or from elsewhere in the body (free flaps). Sometimes, they might also use nerve grafts to help with sensation.
Skin Grafts
Doctors who specialize in rebuilding can fix soft tissue in the tongue, mouth lining, and lips by using a piece of skin called a graft. These grafts can be taken from the belly or leg and used to repair small parts of the mouth lining, known as the mucosa.
Flap Tissue
Sometimes, when big pieces of soft tissue are taken out of the mouth, they can be replaced with healthy tissue called a flap. This flap can be made of skin, muscle, and fat. Flaps can be taken from nearby places like the scalp, cheek, forehead, neck, or chest without cutting off their blood supply. Or, they can be taken from far away parts of the body, which is called a free flap. Surgeons use a special surgery called microvascular surgery to carefully cut and reattach the flap’s blood vessels.
Using a free flap from a distant part of the body gives doctors more choices for finding tissue that fits well in the mouth. Choosing the right tissue can help bring back how the mouth works. For instance, doctors might take skin and soft tissue from the forearm to replace a missing part of the tongue, helping with talking and swallowing.
Nerve Grafts
Doctors might use nerve grafts to help the tongue and lips feel and move better, sometimes also called a tongue replacement surgery. They take a nerve from a part of the body where no one will miss it, and put it where it’s needed in the mouth. This helps with talking and swallowing like normal.
Bone Reconstruction
Before the surgery, specialists take CT scans of the tumor and jaw. They use these scans to make 3D computer models of the areas that need rebuilding. Surgeons then follow these models to help them cut out the cancerous part of the jaw and build a new one.
To fix the jaw, doctors might use a piece of bone from the lower leg called the fibula. They can also fix other bones in the face. For example, they might replace the hard palate, the roof of the mouth, with bone from elsewhere in the body, like the fibula or the shoulder blade.
Doctors make sure that taking bone from one area doesn’t cause problems in that part of the body.
Dental Implants
Once the jawbone is fixed, gum specialists can use dental implants and fake teeth to make your mouth look normal again and let you chew properly.
Dental implants are like tiny screws that go into the upper or lower jawbone to act like a tooth root. They’re made of a metal called titanium, which joins with the jawbone over a few months. Once this is all set, the surgeon adds custom-made fake teeth.
Oral Cancer Reconstructive Surgery Recovery
The time it takes to recover from reconstructive surgery can differ based on the type and extent of the procedure. For small surgeries like skin grafts, patients might only need two to three days in the hospital to recuperate. However, for more complex procedures like replacing a jaw or removing large sections of tissue, the recovery time could extend to a week or longer. It’s important to follow your doctor’s advice and allow yourself enough time to heal properly after surgery.
When you wake up
After your surgery, you’ll likely wake up in the recovery unit or, for bigger surgeries, in intensive care (ICU) or a high dependency recovery unit. You’ll usually return to your ward within a day or so. In the ICU, you’ll have one-to-one nursing care, and in the high dependency unit, you’ll receive very close nursing attention. Your surgeon and anesthesiologist will monitor your progress closely. These units can be busy and noisy, which might feel strange or disorienting for some people. You might feel sleepy due to the anesthesia and pain medication.
Talking after your operation
After surgery on your voice box, mouth, jaw, tongue, or throat, talking might be tricky. It can feel frustrating, like you’ve lost control. But the staff knows about this and they’ll help you out. They’ll put a call bell near you so you can ask for assistance anytime. If you can’t speak, they’ll give you paper and a pen to write down what you need to say. They might also offer you a tablet so you can communicate better while you’re in the hospital.
Painkillers
During the first week after surgery, it’s common to experience pain, but don’t worry, you’ll have painkillers to help. Let your doctor or nurse know right away if you’re in pain so they can find the right painkiller and dosage for you. Taking painkillers regularly is key for them to work best. Right after surgery, you might receive painkillers through a drip you control, called patient controlled analgesia (PCA), or through a thin tube in your back connected to a pump for constant pain relief, known as an epidural.
You’ll also receive painkillers to take home, and your nurse will guide you on when and how to take them, as well as possible side effects. If your pain persists or worsens, contact your doctor promptly.
Eating and drinking
After your operation, whether you can eat or drink depends on the type of surgery you had. If it involves your mouth, you’ll likely not be able to eat or drink for a few days, but you’ll receive fluids through a drip and can moisten your mouth with ice or sips of water. If you have a feeding tube, a dietitian will determine how much liquid feed you need until you can eat and drink normally again.
Once your wound heals, you can slowly increase your intake of fluids. Then, you’ll progress to eating soft foods like soup or jelly. Your dietitian will keep an eye on your progress and reduce your liquid feeds gradually.
Preparation for Oral Cancer Reconstruction Surgery Enhances the Outcome
If you or someone you know is facing oral cancer surgery, understanding the process and what to expect during recovery is crucial. From the initial procedure to post-operative care, there are many aspects to consider, including pain management, communication challenges, and dietary adjustments. Remember to communicate openly with your medical team about any concerns or discomfort you may experience, as they are there to support you every step of the way.
