RCM in Healthcare: The Key to Financial Health in Medical Practices
Managing money well is essential for the success and long-term health of medical practices and hospitals. One key idea that helps with this is Revenue Cycle Management (RCM). So, what is RCM in healthcare, and why does it matter?
What is RCM in Healthcare?
Revenue Cycle Management, or RCM for short, is a financial process that healthcare facilities employ to document everything that happens during a patient’s care, from registration and appointment scheduling to final payment. In simple terms, RCM includes all the administrative and clinical tasks that help manage and collect money for patient services.
The main goal of RCM in healthcare is to make the billing process smoother, reduce mistakes, and ensure that healthcare providers get paid fairly for their services. By using effective RCM processes, medical practices can improve their finances, make patients happier, and spend more time focusing on providing quality care.
Why is Revenue Cycle Management Important?
RCM is not just about billing; it’s a complete system that helps healthcare providers run their business smoothly. Here are some key reasons why revenue cycle management healthcare is crucial:
1. Financial Stability
Recent studies show that 89% of hospitals and health systems have seen more claims being denied, and 86% of those denials could have been avoided. Effective revenue cycle management is critical for keeping healthcare organizations financially healthy. By improving the RCM process, providers can:
- Reduce claim denials
- Minimize billing mistakes
- Improve cash flow
- Reduce the time it takes to collect payments.
These changes lead to more stable and predictable income. This stability allows healthcare providers to invest in better patient care, new technology, and staff training.
2. Better Patient Experience
While RCM mainly focuses on finances, it also helps make patients happier. A well-run revenue cycle can:
- Give patients clear and accurate bills
- Offer easy-to-understand pricing
- Make insurance verification faster
- Reduce billing-related frustrations for patients
By improving these areas, healthcare providers can build trust with their patients and make them more satisfied with the services they receive.
3. Regulatory Compliance
There are numerous rules in the healthcare sector, and breaking any of them might result in major difficulties. A strong RCM system helps healthcare providers:
- Follow coding and billing rules
- Keep accurate records
- Meet reporting requirements
- Protect patient information according to privacy laws
By ensuring they comply with these regulations, healthcare organizations can avoid legal issues and keep a good reputation in the industry.
4. Data-Driven Decision Making
Modern RCM systems provide valuable insights into healthcare businesses’ financial health. This data helps managers to:
- Spot trends in patient demographics
- Analyze which services are profitable
- Find inefficiencies in the billing process
- Make smart decisions about how to use resources
By using this information, healthcare providers can continually improve their operations and adapt to changes in the market.
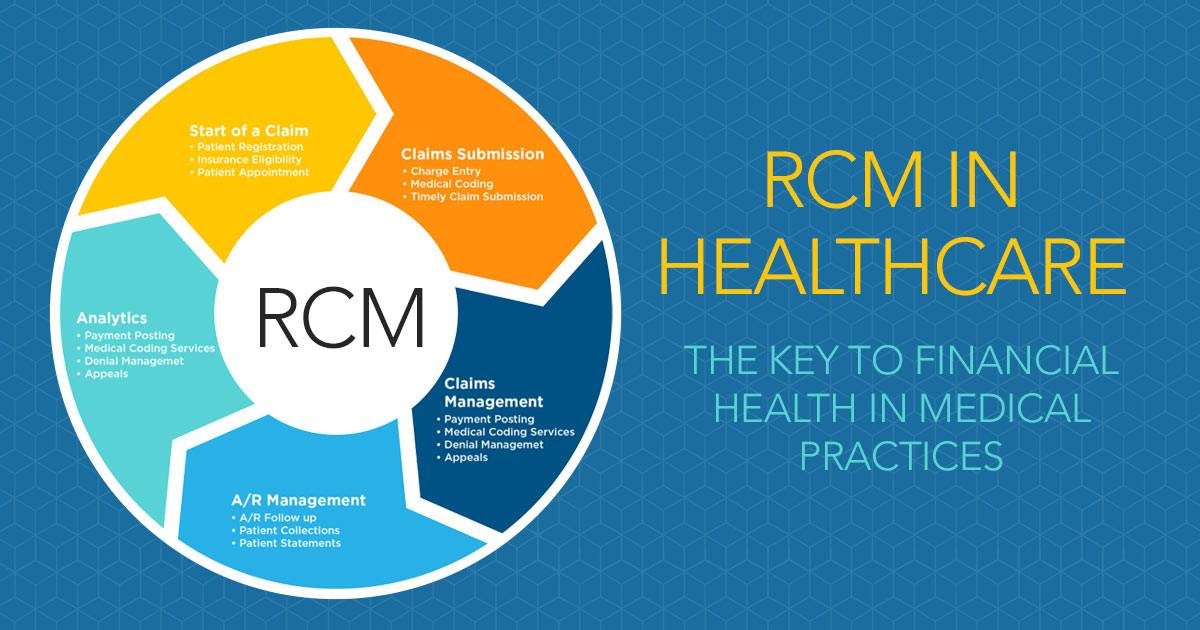
Key Steps in the RCM Process
Understanding the steps of the RCM process helps explain how it works. Healthcare practitioners must complete each step to ensure their compensation for their services.
- Patient Registration and Insurance Verification: The first step is to register the patient and check their insurance coverage. This ensures that the healthcare provider is informed of both the covered services and the patient’s outstanding amount. Accurate insurance verification lowers the chance of future claim denials.
- Medical Coding and Charge Capture: Once a patient has received care, the services offered are translated into medical codes. These numbers are necessary for billing. Healthcare practitioners receive reimbursement for their services when they code accurately.
- Claims Submission: After the medical codes have been allocated, the claim is sent to the insurance carrier. The insurance company completes this online and evaluates the claim to determine its payment amount. Errors in the claim might lead to rejection, thus precision is critical.
- Payment Posting: Following the processing of the claim, the insurance company sends a payment, which the healthcare provider then posts to the patient’s account. If the payment doesn’t cover the entire bill, the remaining balance is billed to the patient.
- Patient Billing: The patient bears the cost of any remaining balance after insurance coverage. In revenue cycle management medical practices, efficient patient billing plays a crucial role in ensuring healthcare providers collect their dues.
- Denial Management: A process determines the reason for a claim’s denial. Common reasons for denials include coding errors or incorrect patient information. Denial management is about fixing these issues and resubmitting the claim.
Best Practices for Effective Revenue Cycle Management
To improve revenue cycle management medical practices, here are a few best practices:
- Automate Processes: Automation can speed up claims submission, payment posting, and patient billing. By eliminating manual labor, healthcare personnel can concentrate on patient care rather than administrative chores.
- Train Staff: Appropriate medical billing and coding training lowers the chance of errors. Regular training is required to ensure that all employees understand the most recent codes and laws.
- Monitor Denials: Keeping track of claim denials can help medical practices spot trends and make corrections early on. Monitoring denials guarantees the resolution of issues before they escalate into significant issues.
- Use Data for Improvement: Regularly evaluating financial data helps to find opportunities for improvement. By tracking metrics like denial rates and payment times, healthcare providers can refine their RCM process.
Challenges in Revenue Cycle Management Healthcare
Managing revenue in healthcare can be complicated. There are several challenges that healthcare providers face in ensuring smooth operations:
- Complicated Billing Processes: Medical billing is complex, with thousands of codes and varying insurance policies. Mistakes can easily occur, leading to claim rejections or payment delays.
- Claim Denials: Claims can be refused for a variety of reasons, including missing information and coding problems. An effective RCM process helps identify the reasons for denials and correct them quickly.
- Regulatory Changes: Healthcare regulations are constantly evolving, and staying compliant can be a challenge. Healthcare providers need to stay updated on new billing and coding standards to avoid penalties.
- Patient Payments: As more patients have high-deductible health plans, collecting payments directly from them is becoming more common. Managing patient billing efficiently is critical to preventing revenue loss.
Why RCM Matters in Healthcare
Revenue Cycle Management (RCM) is crucial for healthcare providers. It helps them manage their finances, improve patient satisfaction, follow rules, and make better decisions. Healthcare organizations can reduce mistakes, expedite payment, and enhance care quality by implementing good RCM practices.
Although there are challenges like complex billing and claim denials, using automation and training staff can help. As healthcare continues to change, a strong RCM process will be important for the success of medical practices and hospitals, allowing them to focus on giving quality care to patients.
